Text “BABY” to 511411
Get FREE tips on your cell phone to help you through your first pregnancy and your baby’s first year.
Powered by Voxiva.
Text4baby is a program of the National Healthy Mothers, Healthy Babies Coalition.
Text “BABY” to 511411
Get FREE tips on your cell phone to help you through your first pregnancy and your baby’s first year.
Powered by Voxiva.
Text4baby is a program of the National Healthy Mothers, Healthy Babies Coalition.
WHAT IS COLIC?

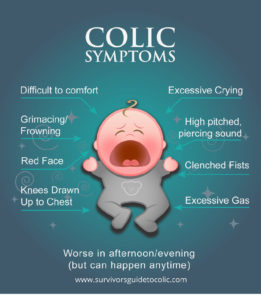
SYMPTOMS:
REMEMBER
There is no cure for colic and there is no known cause, but there are ways to help.
THINGS TO TRY:



IF NOTHING WORKS:
Source: TexasWIC.org
Get To Know Your New Baby: WIC’s Guide for Birth to 3 Months
A New Baby!
You must feel excited and completely overwhelmed!
This booklet will help you learn what your newborn needs to be happy and healthy.
All babies are different, but their movements and noises will let you know when they’re hungry, happy, uncomfortable or just tired.
You will soon learn your baby’s cues and become your newborn’s superhero!
– 1 cup of warm water
– Kitchen Measuring Spoons
– Table Salt
– Nose Dropper
– Bulb Syringe
– Soft Tissues
– A Soft Rolled Up Blanket or Towel
To make the mucous more watery, add saline (salt) water in the nose. To make the salt water drops:
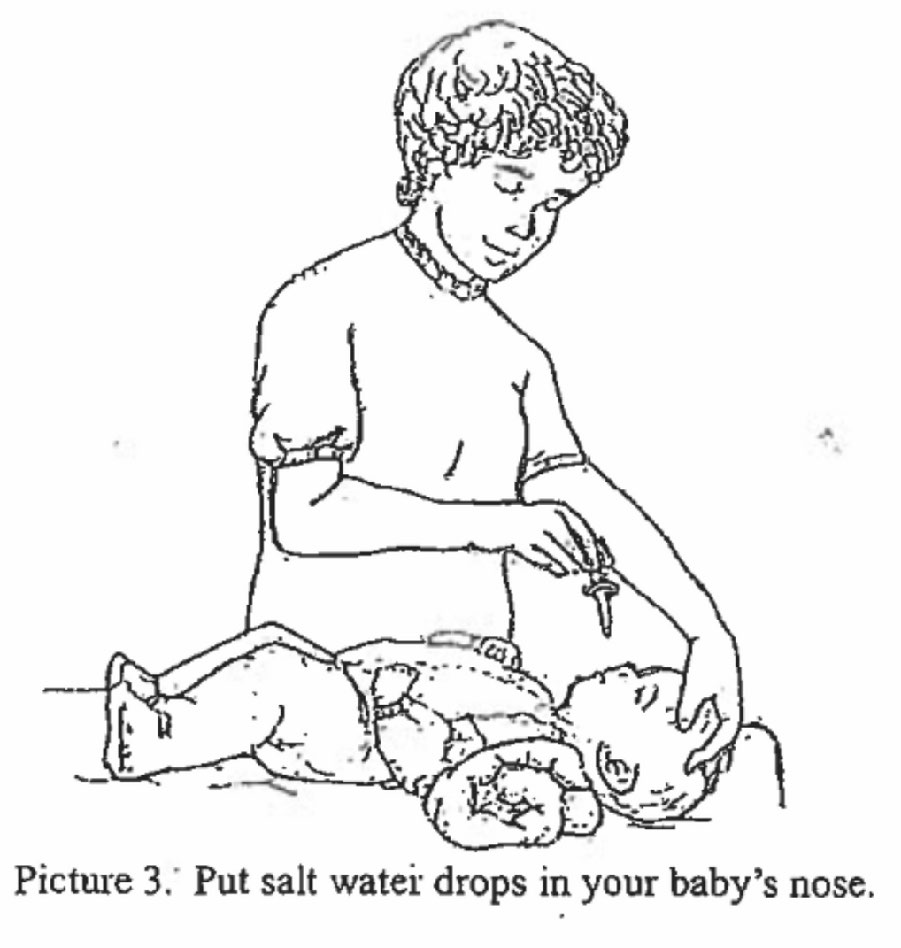

1. Suction your baby before you feed her. If you suction after, the salt water might cause vomiting.
2. To use the bulb syringe, squeeze the air out of the bulb as shown in Picture 4 (above).
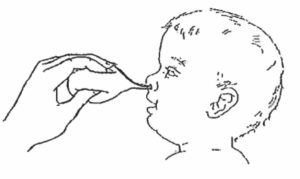
3. While squeezing, gently put the tip of the bulb into on nostril as demonstrated in picture 5 (below).
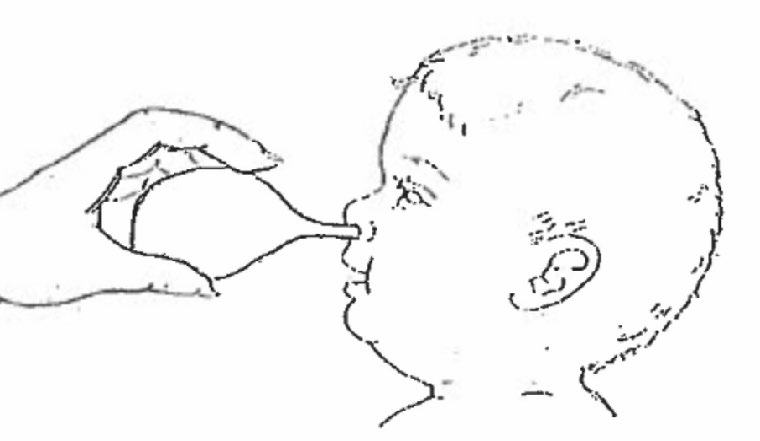
4. Stop squeezing to let the air come back into the bulb. This will pull the mucous out as shown in Picture 6 (above).
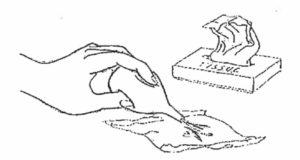
5. Squeeze the mucous out of the bulb onto a tissue as shown in Picture 7 (below).
6. Suction the other nostril the same way.
1. Gently wipe off the mucous around the baby’s nose with tissues.
2. Wash the cup, the dropper, and the bulb syringe in warm soapy water.
3. Squeeze the bulb syringe several times to clean out the mucous. Rinse with clean water.
WHAT IS JAUNDICE?

The newborn on the left does not have jaundice as a yellowish tint is absent.

The newborn on the right has jaundice as seen from the yellowish tint of the skin and eyes.
CAN JAUNDICE HURT MY BABY?
WHAT CAN I DO TO HELP MY BABY’S JAUNDICE GO AWAY?
DOES BREASTFEEDING AFFECT JAUNDICE?
During the COVID-19 pandemic, parents may need to check their children for symptoms, including fever, before they go to school, child care, or sports activities. Feeling your child’s forehead is quick but not very exact. Most modern digital thermometers work fast and are easy to use.
A “normal” temperature varies with the child’s age, activity, and time of day. A fever usually is a temperature of 100.4 degrees Fahrenheit (38 degrees Celsius) or higher. This is a sign that the body is fighting an illness. Your child’s temperature, age and other signs of illness will help your doctor recommend treatment that is best for your child.
Call your pediatrician right away if your child:
What are some different types of digital thermometers?
There are different types of digital thermometers that measure temperature at different areas of the body. Rectal (in the anus) temperatures are the most accurate. Forehead temperatures are the next most accurate. Oral and ear temperatures are accurate if done properly. Armpit temperatures are the least accurate, but you can use this method to screen a child of any age.
Whatever approach is used, follow the cleaning instructions on the package before use.



How to Use a Digital Thermometer
To get the right thermometer reading, it is important to always follow the instructions that came with the device.
Rectal temperature
Taking a rectal temperature gives the best reading, especially for infants under 3 months of age. Here is how to take a rectal temperature:

Oral temperature
 Once your child is 4 years old, you can take a temperature by mouth. Here is how to take an oral temperature:
Once your child is 4 years old, you can take a temperature by mouth. Here is how to take an oral temperature:
Forehead temperature
Temporal artery (forehead) thermometers can be used on children of any age. Here is how to take a forehead temperature:
Ear temperature
Tympanic (ear) thermometers can be used on children 6 months of age and older, as young infants have narrow ear canals. Here is how to take an ear temperature:
Some quick screening ways may not be best
Some products and quick methods are not as accurate at checking a child’s temperature. For example, taking the temperature under the armpit can help schools and child care centers quickly check, but is not very accurate.
Other less accurate ways of checking for fever include using a pacifier thermometer (for children 1 year of age and younger) and fever strips on the forehead. While parents can use them for quick screening, they do not work as well as measuring your child’s rectal, forehead, ear, or oral temperature with a digital thermometer.
Remember
Fever is just one sign of illness, but an important one. Talk with your child’s pediatrician if you have any questions about fever and taking your child’s temperature.
More Information
*Digital thermometer drawings by Anthony Alex LeTourneau.
Last Updated: 10/12/2020
Source: American Academy of Pediatrics (Copyright © 2020)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Help me be healthy.
Before I go home from the hospital, I need:
Find a doctor or nurse to see me for my regular checkups. I need a Medical Home. Bring this calendar to all my checkups. Ask questions, share any worries you have, and work closely with my doctor or nurse to plan all the care I need.
When I go for my first checkup, the doctor will:
Feed me whenever I am hungry.
Breast milk or iron-fortified formula is the only food I need. It will probably take us many weeks to get used to a feeding schedule. This is normal. If I am breastfeeding, I might eat every 2 to 3 hours.
I am getting enough to eat if I am:
Keep me safe.
Whenever we ride in the car, put me in a car seat with the straps on right.
Place me on my back to sleep. Keep my sleeping area clear of stuffed toys and soft, fluffy things.
Keep me safe from fire and smoke.
Pay attention to me. I talk by crying.
If I’m crying, it could mean that I:
Remember, most babies have a fussy time each day. To help me calm down, read “How to Help Your Crying Baby.” The Parents Action for Children website is also helpful.
If nothing seems to help me calm down, check with my doctor to see if something is wrong. Soon you will be able to tell the difference between the cry that says “Feed me” and the cry that says “Pick me up and hold me.”
Play with me. It helps me learn.
Watch how I grow.
Each child grows and changes at a different rate.
Watch the things that I do. If I was born early or have some special needs, it may take me a little longer to do some things. If you are worried about what I can and cannot do, talk to my doctor or nurse.
Watch for me to: